|
FETAL DUODENUM -
NORMAL -
DUPLICATION
CYSTS -
DUODENAL
OBSTRUCTION -
DUODENAL
ATRESIA |
NORMAL ANATOMY |
DUODENAL DUPLICATION CYSTS |
Link to Duodenal Duplication Cysts
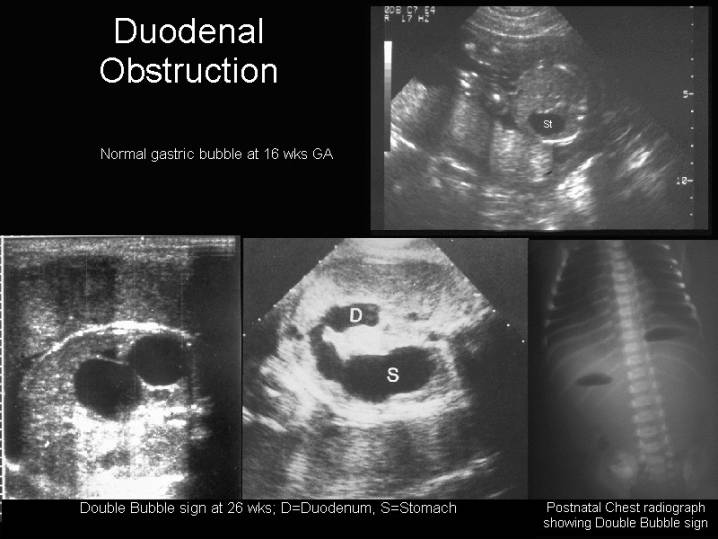
DUODENAL OBSTRUCTION |
Duodenal
obstruction, including both stenosis and atresia, is the most common intestinal
obstruction in newborns and has an approximate incidence of 1 in 10 000 live
births (8). Most obstructions involve the second and third parts of the
duodenum and are located close to the orifice of the bile duct (9), and may be
associated with numerous etiologies (8-13).
Associated congenital anomalies are found in about 50% of the cases and approximately 30% have trisomy 21 (8, 10-16). Familial cases of duodenal obstruction have been reported and a genetic origin has been discussed (8, 14-16).
- Intrinsic atresia (complete or partial failure if canalization)
- Duodenal stenosis / atresia.
- Duodenal web / diaphragms.
- Duodenal duplication.
- Pyloric web or atresia
- Extrinsic compression from annular pancreas, Ladd's bands, volvulus, preduodenal portal vein intestinal duplication or contiguous renal mass.
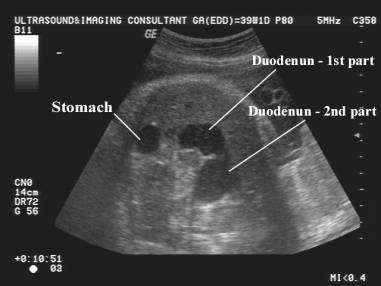
DUODENAL ATRESIA |
- Duodenum is never normally visualized.
- Duodenal obstruction has been reported as early as 14 weeks gestation (1) but is rarely evident before 20 weeks gestation. The diagnosis of duodenal obstruction is rarely made early in pregnancy. This is thought to be due to immaturity of autonomic function resulting in immature gastric emptying (16), Fetal gastric motility is sporadic and infrequent before 20 weeks of gestation. Both gastric motility and gastric emptying significantly increase at around 24 weeks of pregnancy. The mean time of diagnosis in a recent study (22) was rather late in pregnancy (29+2 weeks) and only eight of their cases (28%) were diagnosed before 26 weeks. Any dilatation of duodenum in the second trimester might be abnormal (19) and serial scans may be valuable (20). It has been proposed that the benefits of prenatal diagnosis might justify a routine ultrasound examination also in the third trimester. Even though the diagnosis is rarely made at routine fetal examination in the second trimester, nine out of 11 cases (82%) from the unselected population from the Trondheim area were diagnosed prenatally. Other clinical signs, such as polyhydramnios may raise the suspicion
|
|
- Polyhydramnios (usually of acute onset).
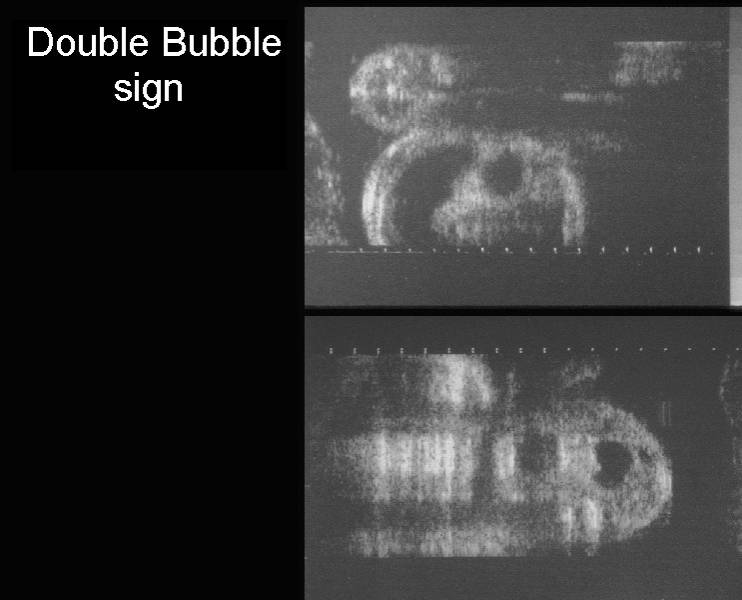
- " Double-bubble"
Sign.
The "double-bubble" sign implies obstruction in the duodenum and although it is most commonly seen in duodenal atresia, it may be found in any of the above causes of duodenal obstruction.
Criteria for diagnosing a Double-Bubble Sign.
Differential Diagnosis of "Double-Bubble" Sign. - Exaggerated peristaltic activity may be present in the region of the obstruction.
|
|
Proximal
Duodenal Atresia – Down Syndrome |
|
|
|
|
|
Duodenal
Atresia – Second part of duodenum -
Normal
karyotype. |
|
|
|
|
|
|
|
Postnatal
Upper GI Series:
|
|
|
|
|
ASSOCIATED ANOMALIES |
- 52-78% have significant associated anomalies (2,3).
- Cardiac defects - 34%.
- Trisomy 21 - 30%.
- Biliary malformations (biliary atresia, choledochal cyst, gallbladder agenesis).
- Malrotation occurs in
up to 40% of cases.
- Esophageal
atresia may be associated with duodenal atresia (7% in one surgical
series) (4).
The combination of both conditions is associated with several other conditions:
1. CHARGE association.
2. VACTERL
association with duodenal atresia (5).
3. Trisomy
21.
4. Feingold
syndrome (oculodigitoesophago-duodenal syndrome) (6):
- Microcephaly, tracheo-esophageal fistula and mesobrachyphalangy.
5. MODED (7): Microcephaly-oculo-digito-esophageal-duodenal syndrome
|
|
|
|
Duodenal atresia and congenital left
sided diaphragmatic hernia (Bochdalek type) |
|
|
|
|
|
|
|
REFERENCES |
- Petrikovsky BM. First trimester diagnosis of duodenal atresia. Am J Obstet Gynecol 1994;171:569-570.
- Grosfeld JL, Rescorla FJ. Duodenal atresia and stenosis: Reassessment of treatment and outcome based on antenatal diagnosis, pathologic variance, and long-term follow up. World J Surg 1993;17:301-309.
- Akhtar J, Guiney EJ.
Congenital duodenal obstruction. Br J Surg 1992;79:133.
- Andrassy
RJ, Mahour GH. Gastrointestinal anomalies associated with esophageal
atresia or tracheoesophageal fistula. Arch Surg 1979;114(10):1125-1128
- Muraji
T, Mahour GH. Surgical problems in patients with VATER-associated
anomalies. J Pediatr Surg 1984;19(5):550-554.
- Courtens
W, Levi S, Verbelen F et.al. Feingold syndrome: report of a new family and
review. Am J Med Genet 1997;73(1):55-60.
- Frydman M, Katz M, Cabot SG et.al. MODED: microcephaly-oculo-digito-esophageal-duodenal syndrome. Am J Med Genet 1997;71(3):251-257.
- Fonkalsrud EW. Duodenal atresia or stenosis. In Bergsma D, ed. Birth Defects Compendium. New York: Alan R. Liss, 1979: 350
- Boyden EA, Cope JG, Bill AH. Anatomy and embryology of congenital intrinsic obstruction of the duodenum. Am J Surg 1967; 114: 190-202
- Kirillova IA, Kulazhenko VP, Kulazhenko LG, Lazjuk GI, Novikova IV. Pancreas annulare in human embryos. Acta Anat 1984; 118: 214-7
- Merrill JR, Raffensberger JG. Pediatric annular pancreas: twenty years' experience. J Pediatr Surg 1976; 11: 921-5
- Young DG, Wilkinson AW. Abnormalities associated with neonatal duodenal obstruction. Surgery 1968; 63: 832-6
- Fonkalsrud EW, de Lorimer AA, Hayes DM. Congenital atresia and stenosis of the duodenum. A review compiled from the members of the surgical section of the American Academy of Pediatrics. Pediatrics 1969; 43: 79-83
- Grosfeld JL, Rescorla FJ. Duodenal atresia and stenosis: reassessment of treatment and outcome based on antenatal diagnosis, pathologic variance, and long-term follow-up. World J Surg 1993; 17: 301-9
- Young DG, Wilkinson AW. Mortality in neonatal duodenal obstruction. Lancet 1966; 2: 18-20
- Lawrence MJ, Ford WD, Furness ME, Hayward T, Wilson T. Congenital duodenal obstruction: early antenatal ultrasound diagnosis. Pediatr Surg Int 2000; 16: 342-5
- Sase M, Tamura H, Ueda K, Kato H. Sonographic evaluation of antepartum development of fetal gastric motility. Ultrasound Obstet Gynecol 1999; 13: 323-6
- Sase M, Nakata M, Tashima R, Kato H. Development of gastric emptying in the human fetus. Ultrasound Obstet Gynecol 2000; 16: 56-9
- Levine D, Goldstein RB, Cadrin C. Distention of the fetal duodenum: abnormal finding? J Ultrasound Med 1998; 17: 213-15
- Nelson LH, Clark CE, Fishburne JI, Urban RB, Penry MF. Value of serial sonography in the in utero detection of duodenal atresia. Obstet Gynecol 1982; 59: 657-60
- Brace RA, Wolf EJ. Normal amniotic fluid volume changes throughout pregnancy. Am J Obstet Gynecol 1989; 161: 382-8
- BrantberAg,
H-G. K. Blaas H-G K,. SalvesenKA et.al. Fetal duodenal obstructions: increased risk of prenatal
sudden death. Ultrasound
Obstet Gynecol
2002; 20: 439